OVERVIEW
Depression is a mood disorder in which a person experiences persistent feelings of sadness and loss of interest. While most people will experience bouts of sadness or irritability from time to time, in depression the sadness lasts longer, for weeks or months, rather than just a few days.
Depression affects how people feel, think, and behave. As a result, depression can cause various emotional and physical problems. The patient may find it difficult to carry out regular daily tasks, and occasionally think that life isn’t worth living. Because depression is more than just a case of the blues, patient cannot immediately “snap out” of it. Long-term treatment may be necessary for depression.
The good news, however, is that with medication, psychotherapy, or both, most people can make a full recovery from depression.
What are the different types and symptoms of depression?
Typically, a person with depression experiences sadness, hopelessness, and a loss of interest in activities that they once enjoyed. There are different types of depression, each having its own specific set of symptoms. The different types of depression may also occur at different times in a person’s life. However, the symptoms of depression can be complicated and differ greatly from person to person. Below are a few common types of depression and their symptoms.
Major Depressive Disorder (MDD)
Major depressive disorder, also known as clinical depression, is a common mood disorder that is characterised by several key symptoms including a depressed mood, a lack of interest in activities that were once enjoyable, changes in weight, changes in sleep, feelings of worthlessness and guilt, difficulty concentrating, and thoughts about death and suicide.
Persistent Depressive Disorder (PDD)
The symptoms of PDD are generally similar to those of MDD. However, PDD is a chronic disorder in which the depressive symptoms come and go over a period of at least two years. And while the intensity of the depressive symptoms can change over time, the symptoms usually do not disappear for more than two months at a time. PDD is also known as dysthymia.
Premenstrual Dysphoric Disorder (PMDD)
A person with premenstrual dysphoric disorder experiences symptoms akin to those of premenstrual syndrome (PMS). However, in PMDD, the symptoms relating to mood are more pronounced. Symptoms of PMDD include extreme fatigue, feelings of sadness and hopelessness, severe feelings of stress or anxiety, mood swings that are often accompanied with bouts of crying, irritability and difficulty concentrating, as well as food cravings or binging.
Seasonal Affective Disorder (SAD)
Seasonal affective disorder’s most common form occurs when a person consistently experiences depressive symptoms during the winter, such as a lack of energy, or changes in their weight, appetite, and sleep patterns, while feeling better during the brighter and warmer seasons.
Postpartum Depression
Postpartum depression affects people who have become parents, including both men and women. Not to be mistaken with the baby blues, the symptoms of postpartum depression are more intense, last longer, and may eventually interfere with the parent’s ability to care for their child or other daily tasks.
The symptoms of postpartum depression usually develop within the first few weeks after the birth of the baby and can last for many months or even longer if left untreated. Common symptoms of postpartum depression include a depressed mood, severe mood swings, excessive crying, difficulties bonding with the baby, withdrawal from family and friends, a loss of appetite, insomnia or excessive sleeping, a lack of energy, a loss of interest in activities that were once enjoyable, intense irritability, feelings of hopelessness, worthlessness or restlessness, and thoughts of harming themselves or the baby.

What are some common misconceptions about depression?
“Depression is a sign of weakness.”
Depression is not a sign of weakness, but a serious medical condition. Hence, depression has nothing to do with a person’s moral character. Instead, it involves a chemical imbalance in the brain, which can be treated by mental health professional. Depression is commonly triggered when a person experiences major life events or changes that can be difficult to deal with, such as the death of a family member or the loss of a job.
“Depression is rare.”
Depression is not a rare medical condition. According to the World Health Organization, an estimated 5% of adults suffer from depression globally. This makes depression one of the most prevalent mental health problems worldwide, a leading cause of disability, and a major contributor to the overall global burden of disease. Anyone can experience depression, regardless of their sex, race or age.

“Depression is temporary and will go away eventually.”
Depression is a medical condition that will not go away if a person does not receive the appropriate treatment and support. Moreover, if treatment is not received, the symptoms of depression will very likely worsen. Therefore, it is crucial to seek help as early as possible to prevent these symptoms from worsening.
“Depression is an untreatable condition.”
According to the World Health Organization, 60–80% of patients respond positively to a combination of medications and psychotherapy treatments for depression. A person with depression can ultimately live a normal and productive life, especially if they receive treatment early. Still, it is crucial to understand that treatment is never instant; a person with depression can take several months and sometimes years to recover.
What are the relationships between depression and anxiety ?
Depression and anxiety are both mental health disorders that are prevalent among the general population. While depression involves feelings of sadness, a low mood, and a lack of interest, anxiety involves intense feelings of stress and worry. Of course, most people will experience bouts of sadness from time to time, and feel worried when faced with stressful and difficult situations. However, persistent or severe feelings of sadness or worry can be symptoms of an underlying mental health disorder. Despite being two distinct disorders, depression and anxiety frequently occur together. For instance, the symptoms of depression can be brought on by an anxiety disorder, such as generalized anxiety disorder or social anxiety disorder. In general, the recommended treatments for depression and anxiety are also similar; both their symptoms tend to improve with a combination of psychotherapy and medications.
If I am experiencing trauma, will depression be triggered?
Depression can be caused by the experience of a deeply distressing or traumatic event. In such cases, it is often the difficulty coping with the painful experience or loss that leads to depression. For instance, survivors of disasters may have lost their homes or loved ones, while survivors of violence or abuse may find it difficult to trust people. Several symptoms of depression also overlap with the symptoms of post-traumatic stress disorder (PTSD), such as difficulties in sleeping and concentrating, and greater irritability. It is also possible for a person to simultaneously suffer from both PTSD and depression.
What are examples of COVID-19-related depression?
The COVID-19 pandemic seriously impacted mental health on a global scale. According to the World Health Organization, in the first year of the COVID-19 pandemic, global prevalence of anxiety and depression increased by a massive 25%. The sharp rise in cases of depression has been linked to the unprecedented stress caused by social isolation throughout the pandemic. Not only can social isolation bring on feelings of loneliness, but it can significantly restrict people’s capacity to work, interact with and receive support from their loved ones, and participate in their communities. Negative life events – such as the suffering or death of a loved one or loss of one’s job – also became more common during the pandemic, placing more people at greater risk of experiencing depression. Among health workers, the mental and physical exhaustion experienced throughout the pandemic was found to be a significant contributor to suicidal thoughts and other depressive symptoms.
How to cope with depression?
Exercise regularly
Regular exercise and a healthy diet can help to improve mood and contribute significantly to the recovery from depression. Exercise can help to boost your self-esteem, lower tension, and anxiety, and stimulate the release of Endorphins, your body’s feel-good chemicals. Exercise can also serve as a useful diversion from any unhelpful or negative thoughts.
Mindfulness and relaxing activities
Sometimes we rush through life without pausing to take notice. You can improve your mental wellbeing with mindfulness techniques that help you to pay attention to the present moment, such as breathing exercises and meditation. Use these activities as an opportunity to become more aware of your thoughts, surroundings, and actions in a purposeful way. Set aside regular times for positive activities that you find help you to relax. This can be anything from reading, drawing, and cooking, to exercising and spending time with friends and family.

Express your feelings
Talk about how you are feeling to people whom you trust such as your family and close friends, instead of bottling up your feelings and attempting to move forward on your own. Try not to avoid activities or places for no reason, and talk to your family and friends about your needs. Help them to help you by letting them know when you are tired, need time out, need a chance to talk or to just be with someone. If you do not feel comfortable discussing your mental health and talking about your feelings with others, you can express your emotions through text or art.
Dos and don’ts for helping individuals with depression
Do:
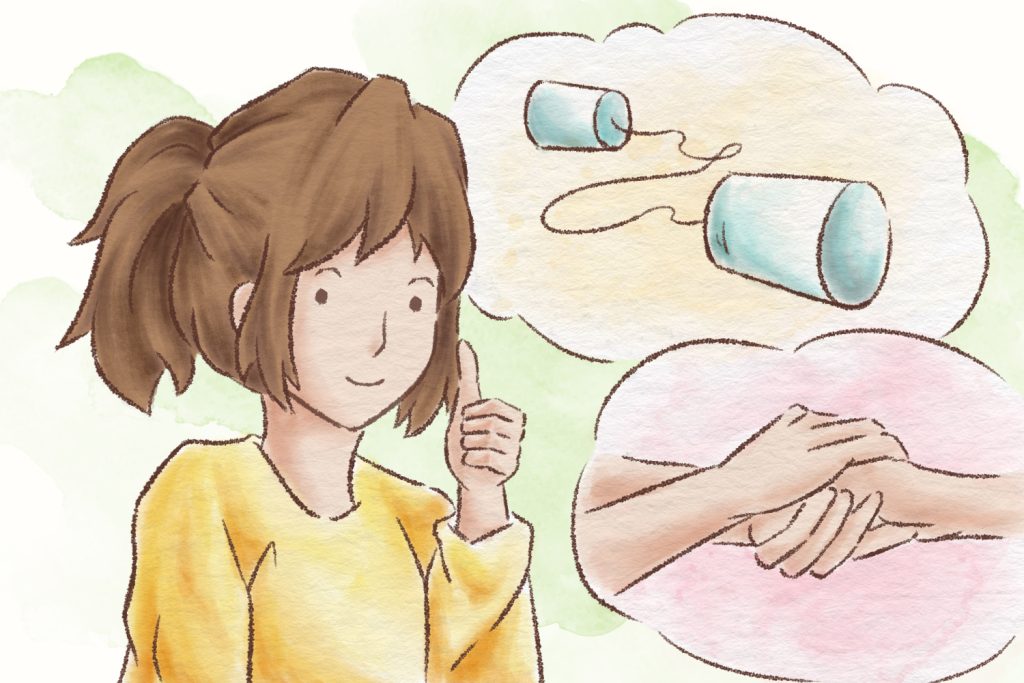
Communicate
Initiate a conversation with the person to genuinely ask them how they are. Use an opening phrase such as “I’ve noticed…” or “I’m worried about…” If you start with “You don’t seem the same…” or “you’ve been acting…” it may cause them to be defensive. You can let the person know that they are not a burden by communicating with them in an honest and empathetic manner.
Show empathy
Imagine yourself in the person’s position, without judgement. Consider how you would feel and how you would want someone to respond if you were experiencing symptoms of depression. Sometimes, lending a sympathetic ear can be of great assistance with eye contact and phrases such as “that sounds challenging, I’m sorry you had to go through this,” and “I’m here for you.”
Support the person to get help
Let the person know that it is absolutely fine to ask for help. Let them know what help is available, but do not force them to get assistance if they do not want to.
Don’t:
Be judgmental
If you have never personally experienced depression, it may be difficult for you to see why someone cannot simply “snap out of it.” The person may already be feeling highly critical of and harsh toward themselves, so it is important not to blame them or pressure them to feel better immediately.
Give up
Depression often cannot be treated quickly or easily. It is important that you are patient and supportive throughout the person’s journey to recovery, however long it may take.
Believe that you can cure them
Treatment for depression can include a combination of medications, psychotherapy, counselling, and lifestyle modifications. As a patient’s treatment needs will ultimately depend on their individual circumstances and symptom severity, it is best to receive therapy of a mental health professional.
If you or your loved ones are experiencing symptoms of depression, it is crucial that you speak to a mental health professional.
CARITAS FAMILY
CRISIS HOTLINE
18288
BAPTIST OI KWAN SOCIAL SERVICE 25354135
Emotional Support and Mental Health consultation hotline
YOUTH OUTREACH HOTLINE
90881023
For youth aged 24 or below
HONG KONG RED CROSS
"Shall We Talk"
(by Appointment Only)
Psychological Support Service

